According to the National Institute of Drug Abuse, “Relapse rates for addiction resemble those of other chronic diseases such as diabetes, hypertension, and asthma.” In numbers, the statistics indicate that anywhere from 40 to 60 percent of people with addiction will experience a relapse, which is very common. In fact, according to the U.S. Department of Health and Human Services, “nearly two-thirds of all relapses occur during the first six months of recovery.”
First of all, it’s important to remember that addiction is a chronic disease. Some people will struggle with relapses their whole life but that doesn’t mean they are a failure or are not actively pursuing their recovery. Setbacks are a reality of recovery for many people because addiction is a lifelong condition that does not have a permanent cure. Despite knowing how to prevent drug addiction relapses, setbacks can still occur.
Recovery is possible for everyone. A healthy way to frame a relapse is to view it as a learning opportunity that teaches how to manage life in sobriety. Ultimately, relapse prevention isn’t only about not drinking or not using drugs. Relapse prevention is about learning new skills and modalities for regulating our emotions and behaviors, and replacing unhealthy behaviors with better habits.
Which drugs have the highest relapse rates?
According to Hazelden Betty Ford, “Users of all drugs are susceptible to relapse, and a person who engages in dysfunctional thoughts or behaviors will be vulnerable to relapse, regardless of their primary drug of choice. Rationalization, minimization and other dysfunctional patterns of thought are not restricted to any one drug. A person may convince themselves that THC is natural and is, therefore, safe. Or they may comfort themselves with the thought that Ativan is a different type of depressant than alcohol and can be used safely. The moral of the story: every drug of abuse will hijack the reward pathways in the brain, and relapse is a threat to anyone in recovery from addiction.
Research shows that alcohol and opioids have the highest rates of relapse, with some studies indicating a relapse rate for alcohol as high as 80 percent during the first year after treatment. Similarly, some studies suggest a relapse rate for opioids as high as 80 to 95 percent during the first year after treatment. Other substances with notoriously high relapse rates are stimulants and benzodiazepines (https://www.hazeldenbettyford.org/articles/relapse-risks-stats-and-warning-signs).”
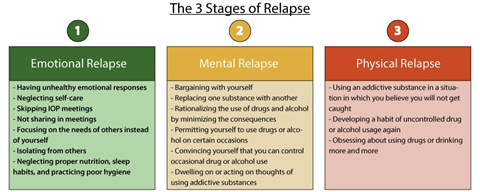
Signs of a Drug Relapse
There are many different physical and behavioral relapse warning signs. Becoming familiar with the signs of relapse can deter someone from using substances again. Some common signs are:
- Drug cravings
- Behavioral:
- Sudden mood changes
- Depressed, anxious, or destructive thoughts
- Denial of events or behaviors
- Secretive behaviors
- Increased irritability
- Relational:
- Avoiding family and friends
- Making impulsive decisions
- Returning to previous habits, routines, or social groups

Common Relapse Risk Factors/Triggers
Drug addiction relapse risk factors/triggers can be stress-inducing people, places or behaviors that can cause someone to misuse drugs or alcohol. Some people get triggered by high-stress situations, but others find celebrations and other positive experiences to do likewise. A person should reflect on their thoughts, feelings and behaviors to learn what triggers them specifically.
Whether relapse factors are verbal, physical, behavioral or environmental in nature, the presence of triggers does not mean that someone will relapse into drug use. With healthy coping mechanisms and a firm resolve, risk factors/triggers can be faced and avoided.

For more info on triggers on how to avoid them: https://www.verywellmind.com/why-did-i-relapse-21900
Why Is Relapse So Dangerous?
The most severe danger associated with relapse is a person’s loss of tolerance, which can easily lead to overdose or death:
- When a person abuses a drug, the brain adjusts and compensates for its effects.
- Once a person stops using, the brain will return to its normal functioning fairly quickly.
- Being sober for a short time can cause tolerance to dissipate quickly.
- If a person decides to use drugs again, even a small or moderate amount can be lethal.
How To Stop a Relapse?
Learning to recognize triggers, getting help from a counselor, creating a relapse prevention plan and building a support network are all useful tools in preventing a relapse and sustaining a healthy, sober lifestyle.
If a relapse happens, it’s much more important to focus on the response rather than fixating on the relapse itself. Most likely, the person already knows why it happened and moving forward in recovery instead is more important than being hindered by it.
1. Take Time for Self-Assessment and Reflection
Recognizing usage patterns to help pinpoint the things that cause a person to resort to substance abuse. Take time to think about how the relapse happened. What took place before the relapse? Did you try to cope in other ways before using? What could you have done instead of using or drinking? The answers to these questions will help you see what you could have done differently and what changes you can make in the future.
If specific cues tend to trigger or create negative emotions, you can create new, healthier habits around them. Generally, there is a sequence to habit forming:
- Cue/Reminder: the trigger that initiates the behavior
- Routine: the reaction to the cue/reminder, and
- Reward: the benefit gained from doing the routine or behavior
By paying attention to the cue or reminder, begin to respond with new routines.
2. Recognize Your Triggers and Warning Signs
A “trigger” is an experience, event or even a person that causes you to stray from a life of sobriety back into substance abuse. Developing an awareness of your triggers and making a list of them can help you actively avoid them on a daily basis. It is helpful to remove yourself from as many triggers as you can, including people, places, and things that remind you of substance use. If some of your triggers cannot be avoided, consider minimizing contact with the trigger immediately after the relapse or at least until you feel more confident in your ability to cope without using.
Create a list:
- Activities I engage in that trigger me (work meetings at a bar, mowing the lawn, etc.)
- Things that often happen to me that trigger me (bills come due, social anxiety, etc.)
- Recovery behaviors that strengthen my emotional and spiritual resolve (meditating, walking the dog, reading)
3. Plan for the Worst
Although this may sound pessimistic, the truth is you don’t want to be stuck without a plan if relapse does happen. A relapse prevention plan is a great tool that can be used to recognize and manage the warning signs and sustain a healthy, sober lifestyle. Write out a step-by-step plan detailing what you will do if you relapse including goals and who will support you in your plan.
- Develop a written relapse prevention plan that outlines:
- Your triggers and warning signs for drug use
- 3 coping skills you know help you deal with stress and urges to use
- People in your support system who you can contact for help
- Local addiction support groups
- Refer to your plan regularly
- Make adjustments over time to keep it relevant to your current life experience
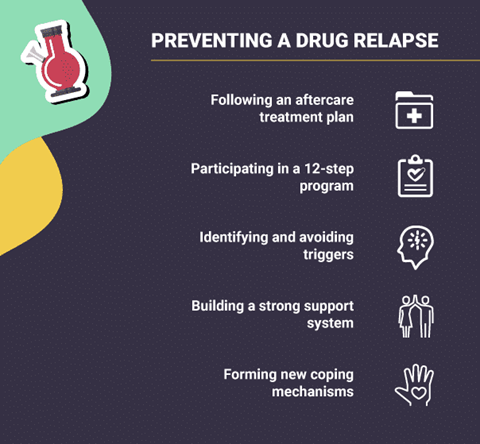
4. Involve Others/Reach Out for Help
Involving other individuals in your recovery is essential to long-lasting change. Make sure you have a few people to call when you experience extreme cravings and/or circumstances. Also make an effort to remove yourself from social situations or harmful relationships that may serve as a trigger.
- Attending a support-help group. Twelve-step groups, such as Alcoholics Anonymous and Narcotics Anonymous, and SMART Recovery, an alternative science-based mutual-help group, can provide a nonjudgmental place to talk about your relapse and an opportunity to learn about how other people have coped with similar situations in the past. There are usually meetings every day, so you should be able to find one the same day as your relapse or within 24 hours.
- Reaching out for help. Seeking support from family, friends, and other sober people can help you cope with a relapse. Surrounding yourself with positive influences can remind you that you are not alone, and sober friends may also provide advice and guidance about how to recover from a relapse.
5. Set Goals for a Healthy Lifestyle
Another very important aspect of a relapse prevention plan is setting daily, weekly, monthly (and forever) goals for achieving a healthy lifestyle. Making daily efforts to prioritize your overall well-being not only helps you manage stress but also reinforces your sense of self-worth and value.
- Setting healthy boundaries. Boundaries are limits that we set for ourselves to protect us from harm. Having weak or poor boundaries can lead to negative emotions, such as anger and resentment, and may pose dangers to your sobriety. Examples of setting healthy boundaries can include refraining from having contact with negative or abusive people and avoiding harmful situations. You can begin by setting boundaries with people who pressure you to use drugs or alcohol.
- Engaging in self-care. Taking care of yourself emotionally and physically is important. Self-care can help you reduce tension and stress and can be any activity that brings you pleasure and does not cause harm, such as yoga, meditation, exercise, reading, journaling, and eating healthy foods.
Do I Need Treatment Again?
The sooner you take steps to intervene following a relapse, the easier it is to get back on track. However, it is never too late to recover from a relapse, so don’t be discouraged if you think you’ve gone too far back into your addiction. It is not uncommon to need professional help to stop using after a relapse; many people benefit from the added support of an addiction treatment program a second and even third time (or more, in some cases).
Similar to other chronic illnesses, relapses during addiction may simply indicate that you need to enter treatment again or adjust the current course of your recovery plan. When deciding whether to attend an inpatient or outpatient program following a relapse, discuss these factors with your treatment team and support system:
Type of drug used. Certain drugs carry a high risk for severe or complicated withdrawal, such as opioids, benzodiazepines, barbiturates, and alcohol. If you relapsed on any of these substances, you may need inpatient detox to safely manage your withdrawal symptoms.
- Quitting opioids, such as heroin, fentanyl, oxycodone, and hydrocodone, can result in very uncomfortable withdrawal symptoms like anxiety, abdominal cramps, nausea, vomiting, and diarrhea.
- Withdrawal from alcohol, benzodiazepines, and barbiturates can be particularly dangerous due to the risk of severe developments such as agitation, delirium, hallucinations, and seizures.
Level of social support. Having a stable sober support system in place at home and in your community plays a role in how you recover from a relapse.
- For those with support at home, an outpatient program may be a good choice, though inpatient options are often suitable as well.
- For those without this kind of help, an inpatient program may be a better option because it provides a more supportive environment.
- Another option may be moving into a sober living facility, which provides structured, drug-free housing. While living there, residents may be expected to follow certain rules and comply with periodic drug testing.
Transportation. Outpatient programs require that participants are able to come and go from the facility as many as 6 days per week. Lack of transportation can make it challenging to commit to these requirements, so if you don’t have a reliable means of transportation, you might opt for an inpatient program.
Physical or mental health conditions. If you have physical or mental health issues in addition to your substance use disorder, you may need the intensity of an inpatient programs since they are often better equipped to treat co-occurring conditions. Women who are pregnant may also be better served in inpatient programs.
Risk for further relapse. Recovering from a relapse is challenging when you are continually faced with triggers, stress, and cravings. While you may be able to stop using temporarily, your chances of returning to substance abuse are high if these issues are not properly addressed.
- Both inpatient and outpatient programs can help you learn how to deal with your triggers, stress, and cravings to reduce the likelihood of a future relapse.
- Less-intensive treatment may be an option if this is your first relapse and you are in good physical and mental health, are not at risk for severe withdrawal, and have a sober support system in place.
Helping a Loved One Avoid Relapse
Friends and family can form an invaluable support network. If you have a friend or family member in recovery, you should be aware of the potential for setbacks and the many ways in which they can occur. This knowledge can help you identify when someone has resumed drug or alcohol use and how to get proper medical help.
How to help someone avoid relapse – some action steps:
- Showing love, support and understanding rather than expressing disappointment and anger
- Avoiding being accusatory about someone’s relapse
- Avoid labeling the person as flawed or at fault for their relapse
- Staying hopeful and optimistic
If someone experiences a relapse, friends and family can:
- Reassure them that they are not a failure
- Remind them that setbacks are common and recovery is an ongoing process
- Help them seek treatment again, if necessary
The possibility for relapse is a reality of recovery. However, relapses are opportunities to create a stronger foundation for the future.
*Medical Disclaimer: The information we provide is not intended to be a substitute for professional medical advice, diagnosis or treatment. It should not be used in place of the advice of your physician or other qualified healthcare provider.
Further Resources:
https://www.drugabuse.gov/publications/drugs-brains-behavior-science-addiction/treatment-recovery
https://www.therecoveryvillage.com/drug-addiction/relapse/
https://americanaddictioncenters.org/treat-drug-relapse
https://www.verywellmind.com/why-did-i-relapse-21900
https://www.hazeldenbettyford.org/recovery/preventing-relapse